Brain cancer prediction in children has taken a significant leap forward, thanks to groundbreaking advancements in artificial intelligence (AI). Recent studies highlight how AI tools can outperform traditional methods in assessing relapse risks among pediatric cancer patients, particularly those with gliomas, a common type of brain tumor. With the ability to analyze multiple brain scans over time, these AI models employ temporal learning techniques to provide more accurate predictions regarding recurrence risk. As researchers continue to refine machine learning algorithms for brain scans, the potential for improving outcomes in pediatric cancer treatment becomes increasingly evident. This innovative approach not only promises better care for young patients but also alleviates the emotional burden on families navigating the complexities of pediatric oncology.
The early detection and forecasting of brain tumors in young patients are emerging as critical areas of research, particularly in the realm of pediatric oncology. Innovative technologies like AI are proving essential in establishing more effective glioma treatment predictions, enhancing our understanding of how childhood brain cancer may progress or relapse. By utilizing advanced methodologies such as temporal learning in medical imaging, healthcare professionals can now assess recurrence risk with unprecedented accuracy. This holistic approach to evaluating brain scans aims to optimize the treatment strategies for children battling cancer, ensuring that those at higher risk receive timely interventions. Ultimately, the integration of such AI-driven solutions promises to revolutionize how we approach and manage brain cancer in the pediatric population.
Understanding Brain Cancer Prediction in Children
Brain cancer in children, particularly pediatric gliomas, presents unique challenges due to their varying recurrence rates. Understanding and predicting these cancer relapses is critical for improving patient outcomes and ensuring timely interventions. Recent advancements with AI models utilized in analyzing intricate details of brain scans provide a glimpse into a future where predictions can be more precise, thereby transforming how we approach pediatric oncology.
The complexity of brain cancer necessitates the application of sophisticated technologies, such as machine learning algorithms, to unearth patterns that are not visible through traditional diagnostic methods. By employing large datasets from numerous pediatric brain scans, researchers can develop predictive models to assess the risk of recurrence effectively. Hence, brain cancer prediction in children is moving toward a data-driven approach that not only enhances diagnostic capabilities but also anticipates treatment needs interactively.
The Role of AI in Pediatric Cancer Treatment
Artificial intelligence is playing a pivotal role in revolutionizing pediatric cancer treatment. Through analyzing vast arrays of MRI scans and integrating temporal learning methods, researchers can generate predictions that enhance our understanding of tumor behavior and treatment results. By focusing on how glioma cases differ in their recurrence risk, AI becomes an indispensable ally in tailoring treatment plans that are both personal and adaptive.
AI’s contribution extends beyond mere prediction; it’s also about improving the overall patient care experience. By minimizing unnecessary follow-ups and invasive procedures, AI tools help alleviate the burden on families during treatment. This innovation means that healthcare providers can confidently identify which patients truly require intensive monitoring, paving the way for more efficient resource management and ultimately better outcomes for young cancer patients.
Temporal Learning in Medical Imaging
Temporal learning represents a significant advancement in the field of medical imaging, enabling AI models to analyze data over time rather than relying solely on single snapshots of a patient’s condition. This approach is particularly useful for tracking the progression or regression of pediatric gliomas, as it allows for more nuanced insight into how tumors develop. By understanding patterns over several months post-surgery, clinicians can better predict the likelihood of cancer recurrence.
The implementation of temporal learning has proven effective, as highlighted by recent studies that demonstrate its superiority over traditional imaging methods. By synthesizing data from multiple MRI scans, the AI tool achieves a predictive accuracy that significantly surpasses that achieved through individual scan analysis. This not only enhances the reliability of recurrence risk assessment but also informs more strategic decision-making in the management of pediatric brain cancers.
Machine Learning Techniques in Brain Scans
Machine learning is reshaping the landscape of diagnostic imaging for brain cancers, especially in pediatric settings. By harnessing algorithms that analyze patterns in brain scans, healthcare providers can gain deeper insights into developing tumor characteristics and treatment responses. The integration of advanced machine learning techniques allows for a comprehensive evaluation of a patient’s medical history and imaging records, facilitating timely and precise interventions.
Moreover, the enthusiasm surrounding machine learning in oncology is buoyed by its potential to improve clinical decision-making. By accurately identifying children at high risk of cancer recurrence, treatment strategies can be tailored more effectively, thereby optimizing outcomes through individualized patient care paths. Through continuous refinement, these intelligent systems are set to revolutionize how healthcare professionals approach brain cancer management.
Recurrence Risk Assessment in Pediatric Gliomas
Understanding the recurrence risk of pediatric gliomas is crucial for developing effective treatment regimens. With tools empowered by AI, assessments can now draw on a plethora of MRI data collected over time, leading to more precise predictions about a patient’s likelihood of relapse. The data reveals subtle changes that may indicate tumor re-emergence, hence facilitating timely adjustments in treatment strategies.
As research continues to evolve, models that assess recurrence risk will become increasingly accurate. The goal is to reduce unnecessary follow-ups and interventions, ultimately sparing children and their families the anxiety and resource expenditure associated with frequent imaging. By integrating advanced technologies into clinical practice, healthcare providers can make informed decisions that prioritize patient well-being while managing the complexities of pediatric glioma treatment.
The Future of AI in Pediatric Oncology
As AI technology continues to evolve, its application in pediatric oncology shows immense promise for improving patient care and outcomes. By developing robust predictive models based on vast datasets, researchers and clinicians are poised to enhance treatment protocols for young patients with gliomas. The integration of AI tools will facilitate more accurate forecasting of treatment responses and recurrence, ultimately paving the way for personalized therapeutic approaches.
Moreover, the goal of implementing AI in pediatric oncology extends beyond mere prediction; it aims to construct a comprehensive framework that supports timely decision-making and enhances quality of life for children battling cancer. Encouraging collaborations among research institutions, healthcare providers, and technology developers will be vital in harnessing the full potential of AI to create transformative solutions in the fight against pediatric brain cancers.
Challenges in Implementing AI in Pediatric Cancer Care
While the benefits of AI in predicting and managing pediatric cancer are extensive, several challenges remain in its implementation. The complexity of developing machine learning models that can accurately assess and predict outcomes based on diverse patient populations must be acknowledged. Additionally, the integration of AI tools into existing clinical workflows can pose logistical challenges, requiring comprehensive training and adjustments for staff.
Another significant concern is ensuring data privacy and security while utilizing sensitive patient information for AI training. Ethical considerations must guide the development and application of these technologies, to foster trust among families and clinicians alike. Addressing these challenges head-on will be essential for the successful incorporation of AI into pediatric oncology, enabling more profound advancements in the diagnosis and treatment of brain cancers.
Clinical Trials and AI in Pediatric Cancer
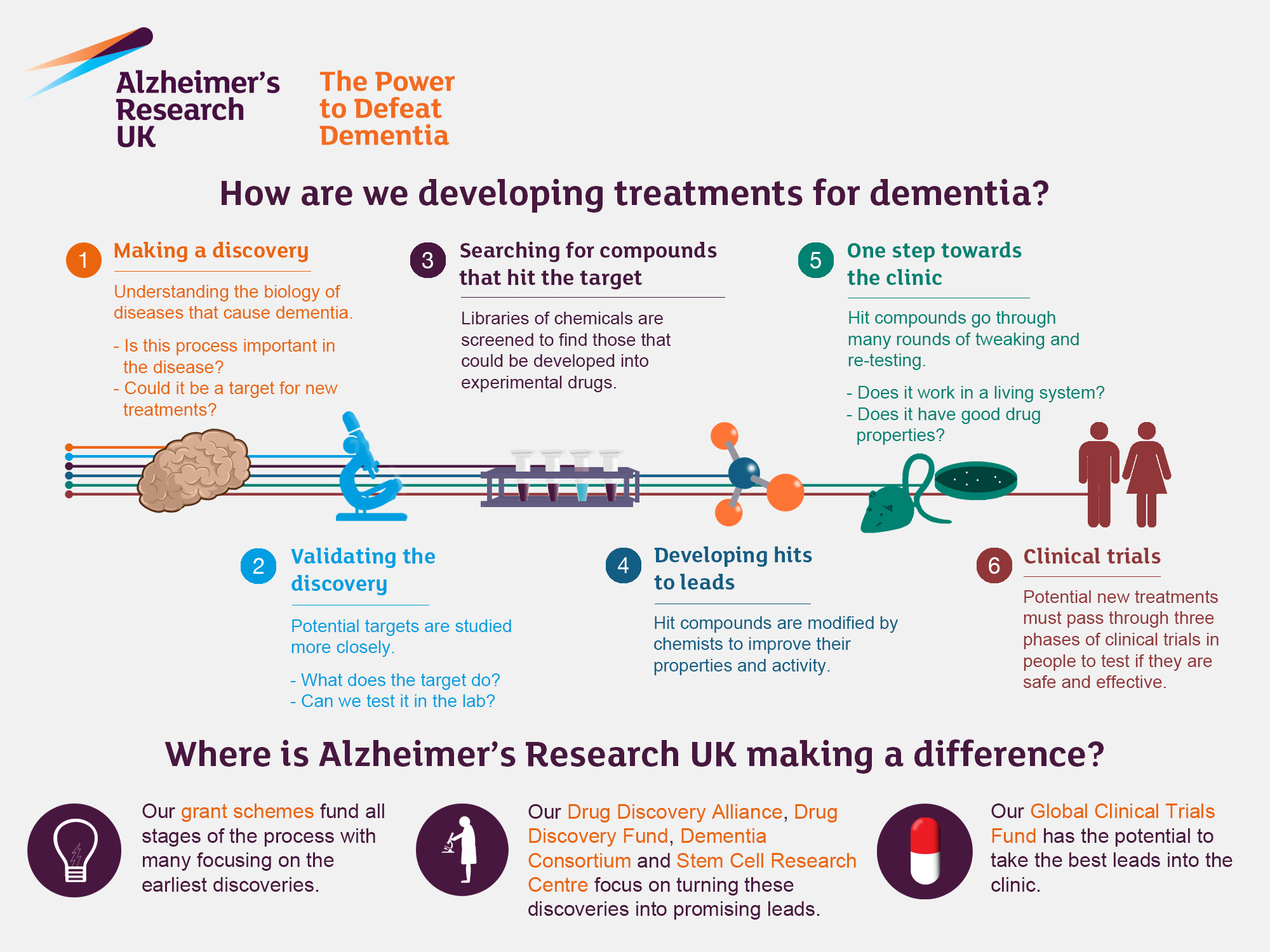
The advent of AI in pediatric oncology opens new avenues for clinical trials aimed at evaluating treatment efficacy and patient outcomes. By employing AI models to predict recurrence risk, researchers can stratify participants more effectively, ensuring that trial cohorts are composed of children most likely to benefit from specific interventions. This targeted approach not only enhances the validity of clinical trials but can also accelerate the approval process for innovative treatments.
Furthermore, leveraging AI-driven insights into recurrence patterns can inform trial design by identifying key endpoints and optimizing treatment protocols. Innovative methodologies involving machine learning could lead to the development of new therapeutic strategies tailored specifically for pediatric glioma patients. As we move forward, the successful implementation of AI in clinical trials will prove pivotal in advancing pediatric cancer care.
Combining Traditional and AI Approaches in Pediatric Oncology
The integration of AI tools alongside traditional methods in pediatric oncology may yield the best outcomes for young patients. While AI provides sophisticated analytical capabilities and predictive accuracy, traditional approaches, such as clinical assessment and caregiver input, remain invaluable for a holistic understanding of a child’s health. Combining these methodologies can create a more comprehensive approach to managing pediatric gliomas.
This hybrid model leverages the strengths of both AI and traditional practices. Clinicians can validate AI predictions with their expertise, ensuring that treatment decisions are made with the utmost care. By fostering collaboration between technology and human insight, we can strive toward delivering superior pediatric cancer care that prioritizes safety, efficacy, and the emotional well-being of patients and their families.
Frequently Asked Questions
What role does AI play in brain cancer prediction in children?
AI plays a crucial role in brain cancer prediction in children by analyzing multiple brain scans over time, significantly enhancing the accuracy of relapse risk assessments. This advanced approach, known as temporal learning, allows for a deeper synthesis of data, improving predictions for pediatric glioma relapse.
How does machine learning contribute to glioma treatment prediction for pediatric patients?
Machine learning contributes to glioma treatment prediction by utilizing advanced algorithms that analyze longitudinal MRI scans from pediatric patients. These models can accurately predict recurrence risks and optimize treatment strategies, enabling tailored care for children suffering from brain tumors.
What is temporal learning in medical imaging, and how does it impact brain cancer prediction?
Temporal learning in medical imaging involves training AI models to recognize changes in brain scans over time, enhancing the prediction of brain cancer recurrence in children. By analyzing sequential MRI images, researchers can identify subtle indicators of relapse that would be missed in single scan assessments.
Why is recurrence risk assessment critical in pediatric glioma treatment?
Recurrence risk assessment is critical in pediatric glioma treatment because it helps identify which patients are more likely to experience a relapse, allowing for timely intervention and tailored follow-up strategies. This proactive approach can significantly improve outcomes and reduce the emotional burden on families.
What are the implications of AI-driven brain scan analysis for children with brain cancer?
The implications of AI-driven brain scan analysis for children with brain cancer include improved prediction of recurrence risks, enabling healthcare providers to personalize treatment plans, reduce unnecessary imaging, and potentially increase the effectiveness of therapies for high-risk patients.
How accurate is the AI tool in predicting recurrence in pediatric brain cancer patients?
The AI tool has demonstrated an accuracy of 75% to 89% in predicting the recurrence of low- and high-grade gliomas one year post-treatment, significantly outperforming traditional methods that only achieve about 50% accuracy based on individual scans.
What future developments can we expect from AI in pediatric cancer care?
Future developments in AI for pediatric cancer care may include clinical trials to validate risk predictions, broad applications of temporal learning in various medical imaging settings, and enhanced treatment protocols based on AI insights, ultimately leading to better outcomes for children with brain cancer.
| Key Point | Details |
|---|---|
| AI Tool Development | An AI tool analyzes multiple brain scans over time for predicting relapse in pediatric cancer patients. |
| Comparison to Traditional Methods | The AI tool provides significantly greater accuracy in predicting relapse risk than traditional imaging methods. |
| Temporal Learning Method | This innovative method allows the AI to learn patterns from scans taken months after surgery, synthesizing data for better prediction accuracy. |
| Accuracy of Predictions | The model predicts glioma recurrence with 75% to 89% accuracy, which is substantially higher than the 50% accuracy of traditional methods. |
| Potential for Improved Patient Care | AI predictions may reduce unnecessary imaging for low-risk patients and suggest targeted therapies for high-risk individuals. |
| Future Research Directions | Further validation in clinical settings is needed before AI can be integrated into regular practice. |
Summary
Brain Cancer Prediction in Children is becoming increasingly effective with advances in AI technology. A recent study revealed that an AI tool utilizing temporal learning methods significantly outperformed traditional relapse risk prediction methods in pediatric patients suffering from gliomas. This breakthrough holds promise for enhancing early identification of at-risk children, improving their treatment outcomes and easing the burden of frequent follow-up imaging. As the research moves towards clinical trials, the goal is to validate these findings and potentially transform patient care in pediatric oncology.